How to Care for Your Child's Feet
It is never normal for a child to experience pain in his or her feet. Foot pain that lasts more than a few days and limits a child’s ability to walk should be examined by a podiatrist. Many adult foot ailments originate in childhood and may be present at birth. Common foot issues that are experienced by children are pediatric flat foot, Sever’s disease, ingrown toenails, and plantar warts.
A child’s foot grows rapidly during the first year, allowing it to reach almost half of their adult foot size. Consequently, foot specialists consider the first year to be the most crucial point in the foot development process. There are ways you can help ensure that your child’s foot develops properly. One way is to carefully look at your baby’s feet. If you notice any deformities, you should immediately seek professional care. You should also loosely cover your child’s foot, since tight coverings may prevent movement and inhibit normal development. Another tip is to change the baby’s positioning throughout the day. If your baby lies down in one spot for too long, it may put an excess amount of strain on the feet and legs.
It is best that you try not to force a child to start walking. Children will begin to walk when they are both physically and emotionally capable to do so. You should also avoid comparing your child’s walking progress with other children because the age range for independent walking may range. When your child’s feet begin to develop, you may need to change both their shoe and sock size every few months to allow room for their feet to grow.
Kids are sometimes prone to splinters, cuts, and severe injuries because they tend to walk around barefoot. This also makes them more susceptible to developing plantar warts which is a condition caused by a virus that invades the sole of the foot through breaks in the skin. These ailments can be avoided by making sure your child wears shoes in unsanitary environments. You should also wash any minor cuts or scrapes on your child’s feet. It is a myth that exposure to fresh air will heal injuries; fresh air will only expose your child’s cuts to germs.
As a parent, you should ensure that your child’s feet are developing properly and are being properly maintained. Consequently, it is important that you perform routine inspections on his or her feet to detect any injuries or deformities in their early stages. Early detection and treatment will help to ensure that your child does not develop any serious foot conditions.
How Simple Foot Exercises Can Help Prevent Falls

As people age, maintaining ankle strength and balance becomes essential for staying mobile and independent. Weakness in the feet and ankles can lead to instability, making everyday movements riskier and increasing the likelihood of falls. Gentle exercises that target the small muscles in the feet and the supportive structures surrounding the ankle can lead to noticeable improvements in strength, coordination, and confidence while walking. These exercises do not require special equipment and can often be done while sitting or holding onto a chair for balance. With regular practice, older adults may find they move with more ease, recover more quickly from stumbles, and feel more secure in navigating uneven surfaces. Strengthening this often-overlooked part of the body plays a valuable role in falls prevention and overall wellness. If you have sustained a foot or ankle injury, or are concerned about balance or ankle weakness, it is suggested that you see a podiatrist.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Bryan Sullivan, DPM from Mississippi Foot Center . Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Jackson, MS . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
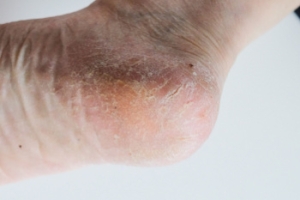
Dry Skin and Cracked Heels
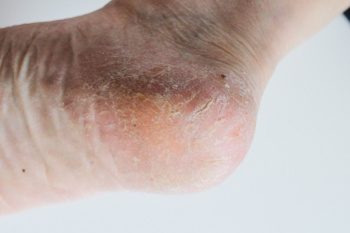
Dry skin on the feet and cracked heels can be uncomfortable and sometimes painful. Lack of moisture is a common cause, as the feet have fewer oil glands compared to other parts of the body. Standing for long periods, wearing open-backed shoes, and walking barefoot can increase the risk of dryness and thickened skin. Risk factors include aging, obesity, and prolonged exposure to harsh weather conditions. Certain medical conditions, such as diabetes, eczema, and thyroid disorders, can also contribute to excessive dryness and cracking. If left untreated, deep cracks may develop, increasing the risk of infection. If you have cracked heels, it is suggested that you consult a podiatrist who can treat this uncomfortable condition, which may include prescribed medication.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Bryan Sullivan, DPM from Mississippi Foot Center . Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Jackson, MS . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Treating Ingrown Toenail Pain

An ingrown toenail occurs when a toenail grows improperly into the surrounding skin, or when the skin around the nail grows too quickly, partially covering the nail. Ingrown toenails often result from improper nail trimming, such as cutting the nail into a curve instead of straight across, or wearing shoes that are too narrow and place excessive pressure on the toes. At first, an ingrown toenail may cause mild discomfort, but as it worsens, the area can become painful, red, and swollen, especially when pressure is applied. If left untreated, infection may develop, leading to pus formation and increased pain. A podiatrist can treat the toenail by gently lifting the edge of it and placing sterile cotton or a flexible tube beneath it to relieve pressure. If the nail is deeply ingrown or infected, this foot doctor may numb the toe and remove the ingrown section to reduce inflammation and prevent recurrence. If you need help with a painful or infected ingrown toenail, it is suggested that you schedule an appointment with a podiatrist for an exam and appropriate treatment solutions.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Bryan Sullivan, DPM of Mississippi Foot Center . Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Jackson, MS . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown Toenail Care
An ingrown toenail is a toenail that grows sideways into the nail bed, causing pain and swelling. Ingrown toenails can worsen and cause drainage, turning into a serious infection.
Several factors affect whether a person is at risk from an ingrown toenail. The many causes include being overweight, diabetes, participating in sports, having a fungal infection of the toe, and cutting your nails too short. Ingrown toenails also have a genetic predisposition, causing some people to be more prone to receive the condition than others. Other causes include improperly fitting shoes and shoes that keep the feet damp.
Ingrown toenails can be preventable with certain measures. For starters, allowing your toe nails to grow slightly longer in length will help prevent them from becoming ingrown. If you have already developed an ingrown toenail, soak the affected toe in warm water. This will alleviate the pain and help prevent an infection from forming. Antibiotic soap or Epsom salts may be added to further help the relieving process and avoid infection. Placing cotton beneath the affected area is also suggested, as this may help the toenail grow upwards and not into the nail bed. Swelling and redness can be reduced by resting with your feet elevated.
A podiatrist should be seen if the pain becomes so serious that it prevents you from doing your everyday activities. If a red streak running up your leg appears or if you suspect your infection has spread, contact a podiatrist immediately. Fast treatments can be undertaken to lessen your pain and have you walking comfortably.
An ingrown toenail can be easily treated with a Band-Aid. Simply wrap the affected toe with a Band-Aid to prevent infection and keep the nail from growing out at a painful angle.
In more serious cases, your podiatrist may decide to make a small incision to remove a portion of your toenail. To prevent the nail from growing back, medication will be placed directly into the nail bed. This procedure would be performed under local anesthesia and is a faster method to alleviate discomfort from an ingrown toenail. Post-procedure directions will have you stay off the affected foot for a day. Afterwards, normal activities can be resumed.
The Importance of Foot Care for Diabetic Patients

Proper foot care is essential for individuals with diabetes to prevent complications like infections and ulcers. Daily inspection of the feet helps identify cuts, blisters, or changes in skin color before they worsen. Washing the feet with mild soap and warm water keeps them clean, while moisturizing prevents dryness and cracking. Toenails should be trimmed straight across to reduce the risk of ingrown nails. Wearing well-fitted shoes with proper support protects against pressure points and injuries. Keeping feet away from extreme temperatures helps prevent burns or frostbite, as complications from diabetes can reduce sensation in the feet. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can help you to manage this serious condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Bryan Sullivan, DPM from Mississippi Foot Center . Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions, please feel free to contact our office located in Jackson, MS . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.